Cutting-Edge Dental Implants: Exploring Advances in Implant Technology
Dental implant technology has evolved dramatically over the past few decades, transforming the way missing teeth are replaced and oral health is restored. Modern advancements have not only improved the durability and functionality of implants but also enhanced their aesthetic appeal and integration with natural bone. From innovative materials to digital planning and guided surgery, cutting-edge dental implants offer patients more predictable outcomes, faster recovery, and a level of comfort that was once unattainable.

Dental implants have revolutionized modern dentistry by providing patients with permanent tooth replacement options that look, feel, and function like natural teeth. As dental technology continues to advance, implant procedures have become more efficient, less invasive, and more successful than ever before. These innovations are making dental implants accessible to a broader range of patients, including those who may have previously been considered poor candidates due to bone density issues or other complications. The cutting-edge developments in implant technology represent a significant leap forward in oral healthcare, offering improved quality of life for those suffering from tooth loss.
Innovative Materials Shaping Modern Implants
The evolution of dental implant materials has dramatically improved both function and biocompatibility. Traditional titanium implants, while still widely used, are now being complemented or replaced by zirconia implants in many practices. Zirconia offers exceptional strength comparable to titanium but with a white color that eliminates the potential for dark lines at the gumline—a significant aesthetic advantage, especially for patients with thin gum tissue.
Surface modifications represent another breakthrough in implant design. Modern implants feature microscopically roughened surfaces that promote osseointegration—the process by which the implant fuses with the jawbone. Some manufacturers have developed implants with nanostructured surfaces that mimic the natural bone matrix, encouraging faster and more complete integration. These surfaces may be treated with bioactive coatings containing growth factors or antimicrobial properties that reduce infection risk while accelerating healing.
The latest generation of implants also includes designs that preserve more bone tissue during placement. Platform-switching technology, where the implant-abutment connection is moved inward from the edge of the implant, has been shown to maintain bone levels around the implant crest more effectively than traditional designs. This advancement helps maintain gum health and aesthetic outcomes over the long term.
Digital Planning and Guided Implant Surgery
The integration of digital technology has transformed the implant planning and placement process. Cone Beam Computed Tomography (CBCT) scans provide detailed 3D images of a patient’s oral anatomy, allowing dentists to precisely plan implant placement before surgery. This technology enables practitioners to identify potential challenges, such as insufficient bone volume or proximity to nerves, and develop solutions beforehand.
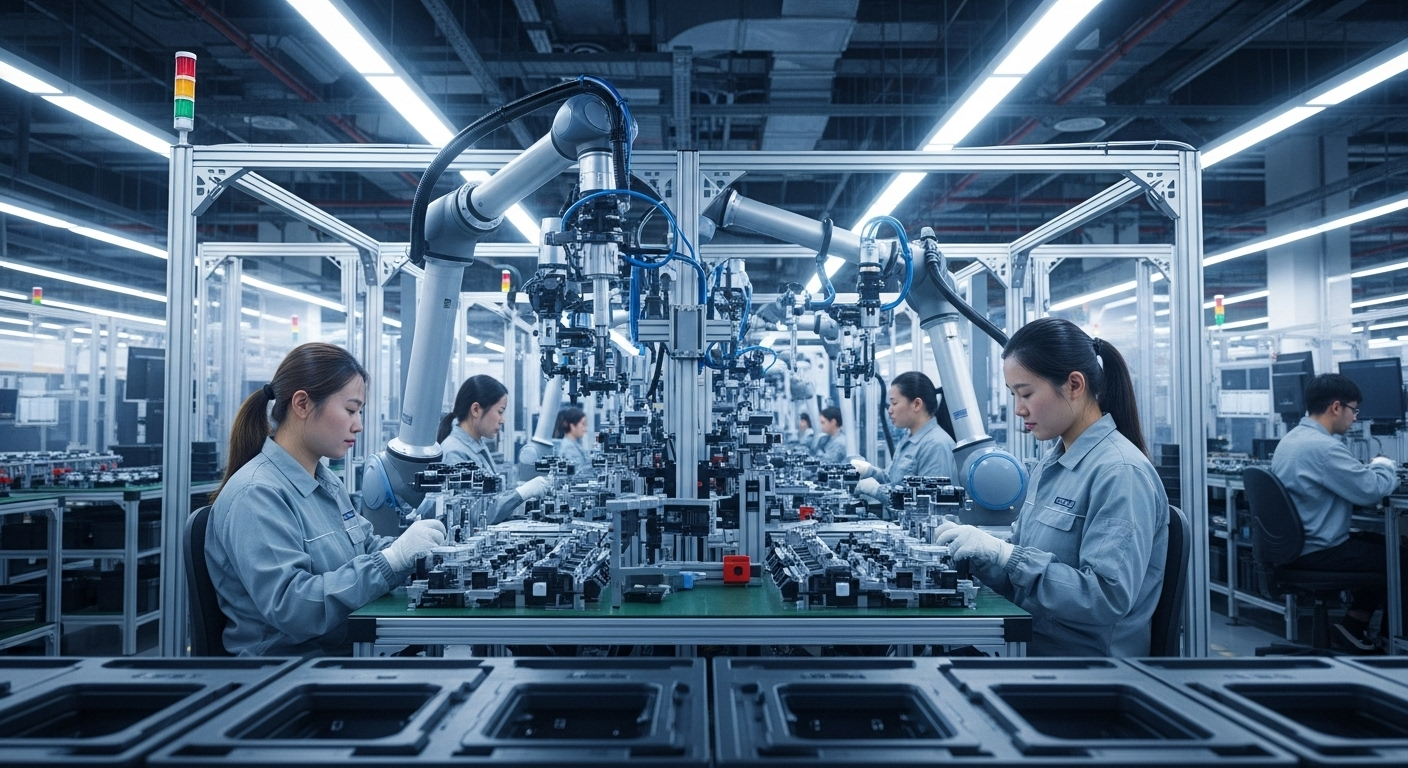
Computer-guided surgery has elevated precision to unprecedented levels. Using specialized software, dentists can virtually place implants in optimal positions and then transfer this plan to the surgical environment using custom-made surgical guides. These guides direct the exact position, angle, and depth of each implant, minimizing human error and reducing surgical time. Some advanced systems even offer real-time navigation during surgery, similar to GPS technology, allowing for adjustments if needed.
Digital impression systems have eliminated the need for uncomfortable traditional molds. Intraoral scanners capture detailed images of the oral cavity, which are used to design perfectly fitted prosthetic components. CAD/CAM (Computer-Aided Design and Computer-Aided Manufacturing) technology then fabricates these components with exceptional accuracy, often in a single appointment. This digital workflow not only improves precision but also significantly reduces the number of visits required to complete treatment.
Enhanced Healing and Patient Comfort
Modern implant systems incorporate design features specifically aimed at improving the healing process and patient experience. One significant advancement is the development of implants with progressive thread designs that provide immediate stability upon placement. This initial stability, known as primary stability, is crucial for successful osseointegration and allows for faster loading protocols in many cases.
Platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) therapies represent biological approaches to enhancing the healing process. These techniques use components from the patient’s own blood to create concentrated growth factor preparations that are applied to the surgical site. Studies have shown these preparations can accelerate tissue regeneration, reduce inflammation, and minimize post-operative discomfort.
Minimally invasive surgical techniques have also transformed the implant experience. Flapless surgery, where implants are placed through small punctures rather than large incisions, reduces tissue trauma and post-operative swelling. This approach preserves blood supply to the area, potentially speeding healing and reducing discomfort. For patients requiring bone augmentation, newer grafting materials with enhanced regenerative properties are available, some derived from the patient’s own cells to maximize compatibility and success rates.
Advanced Diagnostic and Monitoring Technologies
The evolution of diagnostic technologies has significantly improved implant planning and long-term monitoring. Digital smile design software allows patients to preview their expected results before treatment begins, facilitating better communication between patients and practitioners about aesthetic goals. This technology integrates with treatment planning software to ensure functional and aesthetic outcomes align.
Emerging technologies such as resonance frequency analysis provide objective measurements of implant stability throughout the healing process. These devices allow practitioners to monitor osseointegration non-invasively and make evidence-based decisions about when to proceed with final restorations. Some systems even permit remote monitoring, enabling dentists to track implant health between appointments.
Artificial intelligence is beginning to play a role in implant dentistry as well. AI algorithms can analyze radiographic images to help identify optimal implant positions, detect early signs of potential complications, and even predict treatment outcomes based on patient-specific factors. While still developing, these technologies promise to further personalize implant treatment and improve success rates.
The Future of Dental Implant Technology
Looking ahead, several promising technologies are on the horizon for dental implants. Bioactive implant surfaces that actively promote bone growth and fight infection represent one exciting area of research. These surfaces may incorporate antimicrobial nanoparticles or be designed to release growth factors gradually during healing.
3D printing technology is poised to revolutionize implant manufacturing. Custom-designed implants that precisely match a patient’s anatomy could become standard practice, potentially improving integration and functional outcomes. Some researchers are exploring 3D-printed implants made from bioresorbable materials that would gradually be replaced by natural bone tissue.
Perhaps most revolutionary is the field of tissue engineering, where scientists are working to develop biological tooth replacements grown from stem cells. While still experimental, this approach could eventually provide patients with completely natural replacement teeth that develop their own blood supply and periodontal ligament—features that even the most advanced current implants cannot offer.
This article is for informational purposes only and should not be considered medical advice. Please consult a qualified healthcare professional for personalized guidance and treatment.